Articles by Jaime Rosenberg

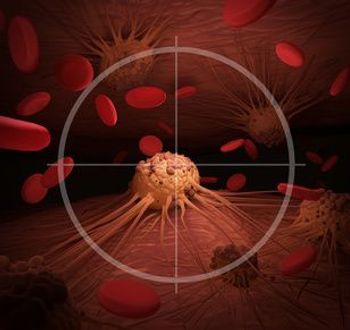
Previous research has suggested the efficacy of chimeric antigen receptor natural killer (CAR-NK) cells in hematological malignancies, and more recently, preclinical findings have raised the question of whether the type of treatment could be a viable, potentially more attractive option for solid tumors.

Researchers outlined novel approaches to prevent and manage cytokine release syndrome (CRS), which occurs frequently in patients receiving chimeric antigen receptor T-cell therapy.
There are no curative treatments for Tangier disease, but gene therapy for ABCA1 has been highlighted as a potential avenue for treating the disease, say the researchers of the paper.

According to researchers, the findings suggest that receiving ibrutinib improves the activity of anti-CD19-CAR T cells.
Strategies for improving outcomes across hematologic cancers and solid tumors range from addressing cytokine release syndrome and neurotoxicity mediators, immune rejection, on-target off-tumor toxicity, post-infusion control limitation, and immunosuppressive tumor microenvironment.

As more therapies continue to be approved, efforts will focus on toxicity prevention and mitigation strategies for associated unique and potentially life-threatening adverse reactions.

While these therapies continue to revolutionize the treatment landscape of SMA, treatments are not without shortcomings or challenges.

In a new review, researchers outline both the underlying pathological mechanisms and potential therapeutic targets in pulmonary arterial hypertension (PAH).
The compiled results revealed that hepatotoxicity related to the gene therapy typically presented as cholestatic, which could be prophylactically treated with prednisolone.

A year after the FDA approved Zolgensma for the treatment of spinal muscular atrophy in children aged under 2 years without end-stage weakness, researchers shared safety and early efficacy data from the first 21 children treated with the gene therapy in Ohio.
While the results are early, if further research proves the approach effective, it could help boost the impact of treatments like chimeric antigen receptor (CAR) T-cell therapy, which to date hasn’t had much luck in solid tumors.

AveXis—a Novartis company—announced that it will work with payers to implement 5-year outcomes-based agreements and novel pay-over-time options. The company also said it will offer a patient program to support affordability and access.
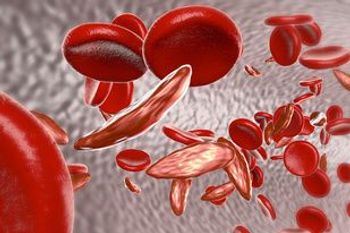
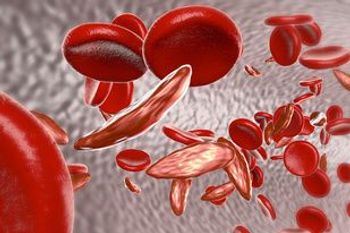
Voxelotor, a first-in-class oral therapy, is both safe and effective in sickle cell disease, according to a phase 1/2 randomized study assessing the drug. These findings were consistent across all doses, ranging from 500 to 1000 mg.
Study results demonstrated that in adult patients with blastic plasmacytoid dendritic cell neoplasm, the targeted therapy resulted in high response rates, particularly among treatment-naïve patients.

As part of CMS’ FY 2020 Medicare Hospital Inpatient Prospective Payment System and Long-Term Acute Care Hospital Prospective Payment System Proposed Rule and Request for Information, the agency is proposing an increase in how much it reimburses hospitals for chimeric antigen receptor (CAR) T-cell therapy, as well as wage index hikes for rural hospitals.

We've rounded up the top 5 most read articles of June, including trial results from the 2018 American Society of Clinical Oncology Annual Meeting and a FDA breakthrough therapy designation for a gene therapy.

Tisagenlecleucel, sold as Kymriah, has gained its second indication following the FDA's approval of the chimeric antigen receptor T-cell therapy for the treatment of adult patients with relapsed or refractory large B-cell lymphoma, the most common form of non-Hodgkin lymphoma.

While calcitonin gene-related peptide (CGRP) inhibitors are projected to have a positive impact on the health of patients with chronic or episodic migraines for whom preventive therapy had failed relative to no treatment, it is likely that the inhibitors will exceed commonly-cited willingness-to-pay thresholds, according to a report from the Institute for Clinical and Economic Review (ICER).
CAR T-cell therapies tisagenlecleucel (Kymriah, Novartis) and axicabtagene ciloleucel (Yescarta, Kite Pharma/Gilead) may come with hefty price tags, but the cost-effectiveness of both therapies fell below or within commonly cited thresholds of $50,000 to $150,000 per quality-adjusted life years, according to a report by the Institute for Clinical and Economic Review.

From 2002 to 2015, CD4 cell counts at the start of combination antiretroviral therapy (cART) increased, and the proportion of individuals with severe immunodeficiency at the start of cART decreased among all income groups, according to a study published in Clinical Infectious Diseases.
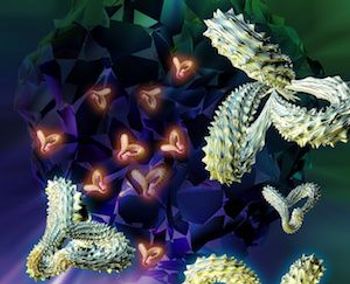
Chimeric antigen receptor (CAR) T-cell therapy has been named the Advance of the Year in ASCO’s Clinical Cancer Advances 2018. According to the annual report, CAR T-cell therapy is “poised to transform the outlook for children and adults with certain otherwise incurable cancers."

Eisai’s multiple receptor tyrosine kinase inhibitor lenvatinib and Merck’s anti–PD-1 therapy pembrolizumab as a combination therapy for patients with renal cell carcinoma received the designation based on results from the renal cell carcinoma cohort in Study 111.

While chemotherapy with thoracic radiation has been established as the standard of care for the initial treatment of non-metastatic small-cell lung cancer, a large proportion of patients do not receive these treatments and in turn have lower overall survival, according to a study published in JAMA Oncology.