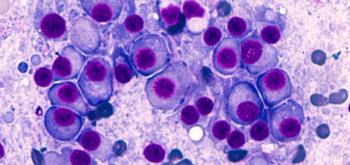
In 37 evaluable patients, the objective response rate in the study was 89% (95% CI, 75%-97%) with complete responses in 78%.
In 37 evaluable patients, the objective response rate in the study was 89% (95% CI, 75%-97%) with complete responses in 78%.
In this late-breaking poster presented at the Tandem Meetings, investigators recommend that patients with primary or secondary central nervous system lymphoma be included in future clinical trials for CAR T-cell therapy.
Armed with an average of 14.3 months of follow-up data, investigators share updates from a cohort in the phase 2 study evaluating cilta-cel in lenalidomide-refractory patients with progressive multiple myeloma after 1-3 prior lines of therapy at the 2022 Tandem Meetings.

Treatment with the first-generation precision cell therapy Orca-T led to a significant reduction in cases of graft-versus-host disease, an impressive GVHD relapse-free survival rate, a lack of treatment-related mortalities, while showcasing scalability potential.
The HSPC therapy showed fetal hemoglobin production in transfusion-dependent patients in a matter of months—with sustained results over 1 year.

Treatment with the investigative gene cell therapy betibeglogene autotemcel led to durable transfusion independence in 87% of pediatric patients less than 18 years of age with transfusion-dependent beta-thalassemia with a median average hemoglobin of 11.3 g/dL.
Responsiveness to treatment received immediately prior to CAR T-cell therapy may not be associated with post–CAR T outcomes in patients with relapsed/refractory diffuse large B-cell lymphoma who receive axicabtagene ciloleucel.