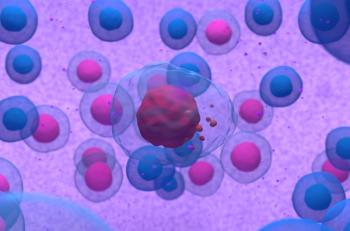
CAR T-cell therapy use will likely expand to a wider array of hematologic malignancies.
CAR T-cell therapy use will likely expand to a wider array of hematologic malignancies.
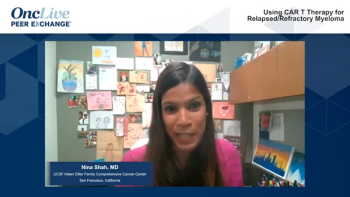
Nina Shah, MD, and other experts discuss the role of CAR T-cell therapy in relapsed/refractory multiple myeloma.
Iuliana Vaxman, MD, and Angela Dispenzieri, MD, review eligibility criteria for ASCT in AL amyloidosis, conditioning dosing, efficacy in terms of hematologic and organ response, and future areas of research.
The FDA previously approved ide-cel as the first BCMA-directed CAR T-cell therapy for patients with relapsed/refractory multiple myeloma following 4 or more prior lines of therapy.

Kelly Garvin, BSN, RN, OCN, discussed methods to communicate the benefits and risks of CAR T-cell therapy to patients and recognize AEs.

The chief scientific officer and chief medical officer of Ultragenyx Gene Therapy discussed the company’s future research in gene therapies.
Mustang Bio plans to file an IND and start a phase 1 clinical trial as soon as a lead construct is identified.
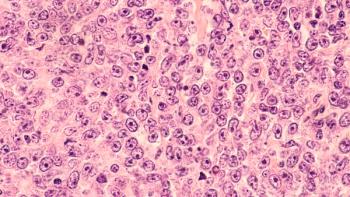
Investigators sought to understand the mechanisms of transferred T cell proliferation and expression.

Jennifer Buell, PhD, president and chief operating officer of Agenus, discussed the VISION platform the company uses to develop therapies.
Krina K. Patel, MD, MSc, discussed moving away from chemotherapy and toward immunotherapy.

With a new paradigm of treating previously incurable diseases comes a new pay paradigm for million-dollar therapies.

Kevin Heller, MD, executive vice president of research, Jasper Therapeutics, discussed future research with JSP191.
Julie Vose, MD, professor of internal medicine and division chief, Division of Oncology and Hematology, University of Nebraska Medical Center, discussed the use of CAR T-cell therapy in non-Hodgkin lymphoma.
The ongoing phase 1 UNIVERSAL trial has demonstrated an overall response rate of 60% among 10 patients.

Rocket Pharmaceuticals plans to quickly resume the phase 1 trial and commence dosing in their new, low-dose, pediatric cohort in Q3 2021.

The chair of the Lymphoma Group at Mayo Clinic discussed incorporating immunotherapies beyond CAR T-cell therapy in non-Hodgkin lymphoma.

Targeted CRISPR therapy has potential in treating inherited retinal diseases.

The professor from the University of Texas Anderson Cancer Center discussed challenges surrounding CAR T-cell therapy for the treatment of follicular lymphoma and other lymphomas.

The professor and chief, of oncology and hematology at University of Nebraska Medical Center discussed research with CAR T therapy in lymphoma.

A phase 1/2 study evaluating Vivet Therapeutic’s VTX-801 is set to initiate in August 2021.

Magali Taiel, MD, chief medical officer, GenSight Biologics, discussed the company’s work in ophthalmic diseases.
David G. Maloney, MD, PhD, covered the importance of standardized criteria in managing CRS and ICANS with CAR T therapy.

The chief executive and chief medical officer of Celyad Oncology discussed the advantages of allogeneic CAR T therapies over autologous ones.

The executive director of the Steele Center for Translational Medicine at the Moran Eye Center discussed the research his team has been conducting in AMD.

The World Federation of Hemophilia’s registry will include long-term safety and efficacy data in people with hemophilia treated with gene therapies.

The professor of clinical medicine, director, Multiple Myeloma and Amyloidosis Program, New York-Presbyterian Hospital, discussed utility of cellular therapies in multiple myeloma.

Experts discuss the use and selection of CAR T therapies in relapsed/refractory diffuse large B-cell lymphoma.

Salvador Rico, MD, PhD, chief medical officer, Encoded Therapeutics, discussed the company’s gene therapy pipeline, including their lead program ETX101.

Bluebird Bio’s latest clinical hold follows another report of MDS in a treated patient.

Despite setbacks in DME, Adverum Biotechnologies said it will continue to develop ADVM-022 for wet AMD.