
Catch up on the latest news, breakthroughs, and announcements from biotechnology companies making advancements in cell and gene therapies.

Catch up on the latest news, breakthroughs, and announcements from biotechnology companies making advancements in cell and gene therapies.

Catch up on the latest news, breakthroughs, and announcements from biotechnology companies making advancements in cell and gene therapies.

Catch up on the latest news, breakthroughs, and announcements from biotechnology companies making advancements in cell and gene therapies.

Catch up on the latest news, breakthroughs, and announcements from biotechnology companies making advancements in cell and gene therapies.

Catch up on the latest news, breakthroughs, and announcements from biotechnology companies making advancements in cell and gene therapies.

Catch up on the latest news, breakthroughs, and announcements from biotechnology companies making advancements in cell and gene therapies.

Catch up on the latest news, breakthroughs, and announcements from biotechnology companies making advancements in cell and gene therapies.
Kadimasem’s lead clinical candidate, AstroRx, was recently cleared for trials in the US for people with ALS.

Catch up on the latest news, breakthroughs, and announcements from biotechnology companies making advancements in cell and gene therapies.
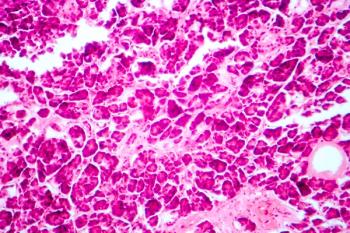
The trial has completed enrollment and all 14 patients have demonstrated islet cell engraftment and endogenous insulin production.

Catch up on the latest news, breakthroughs, and announcements from biotechnology companies making advancements in cell and gene therapies.
These, among many others, are some of the key clinical trials of gene, cell, and regenerative therapies that the CGTLive staff will be following throughout 2024.

Take a look at the stories that stood out as pillars of progress and success in endocrinology gene and cell therapy development in 2023.

Catch up on the latest news, breakthroughs, and announcements from biotechnology companies making advancements in cell and gene therapies.

Take a look at the stories that stood out as pillars of progress and success in endocrinology gene and cell therapy development in 2023.

Catch up on the latest news, breakthroughs, and announcements from biotechnology companies making advancements in cell and gene therapies.

Catch up on the latest news, breakthroughs, and announcements from biotechnology companies making advancements in cell and gene therapies.

Catch up on the latest news, breakthroughs, and announcements from biotechnology companies making advancements in cell and gene therapies.

Catch up on the latest news, breakthroughs, and announcements from biotechnology companies making advancements in cell and gene therapies.
One patient had their Cell Pouch removed after the donor islet cells were found to be contaminated with Candida albicans yeast.
The director of the Center for Immunity and Immunotherapies at Seattle Children's Research Institute discussed preclinical research on overcoming limitations of Treg cells through genetic engineering.
All patients showed improved glycemic control and a reduction in insulin independence.

The phase 1/2 trial features 3 phases, with new sites expected to open in the coming months. VX-264 uses the same stem cell-derived islets used in the VX-880 program in type 1 diabetes.
The 2 patients were among 6 who have received treatment in Vertex’s trial so far and were the only 2 evaluable for the primary efficacy end point.
Five patients in the cohort achieved this milestone and Sernova noted a sixth patient in the cohort is still awaiting assessment of islet graft function.