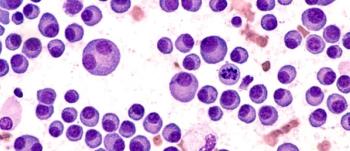
Real-world data showed ide-cel was active in patients with central nervous system manifestations of multiple myeloma.
Real-world data showed ide-cel was active in patients with central nervous system manifestations of multiple myeloma.

The head of the Referral Center for Sickle Cell Disease and Clinical Research Department at Hôpital Intercommunal de Créteil of the Université Paris Cité discussed the Drepagreffe-1 and 2 studies and improvements seen over 10 years of follow-up.

The associate director of clinical in vivo gene therapy at Children’s Hospital of Philadelphia discussed follow-up data of up to 6 years with investigations of fidanacogene elaparvovec.

The clinical director of lymphoma services at the University of Colorado discussed 5-year follow-up data from the TRANSCEND-NHL-001 clinical trial.

Haydar Frangoul, MD, the medical director of pediatric hematology/oncology at Sarah Cannon Research Institute and Pediatric Transplant and Cellular Therapy Program at TriStar Centennial, discussed the latest data update from the CLIMB SCD-121 trial evaluating exa-cel.
The results come from patients with lenalidomide-refractory MM treated in the CARTITUDE-4 trial after 1 to 3 lines of prior therapy.

The professor of pediatric hematology/oncology at CS Mott Children’s Hospital discussed findings from the open-label extension of the ATLAS studies at ASH 2024.

A long-term follow-up to the DREPAGREFFE-1 trial suggest that children with sickle cell anemia may benefit long-term on risk of cerebral injury, cognitive functions, and quality of life over standard care transfusions.

Among those who had undetectable minimal residual disease, autologous hematopoietic cell transplantation showed signs of benefit only for those who remained MRD-positive following induction therapy.

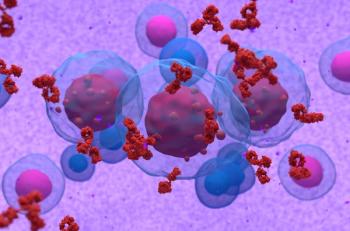
Arlocabtagene autoleucel shows promise as a potential first in class GPRC5D-targeted CAR T-cell therapy for heavily pretreated multiple myeloma.
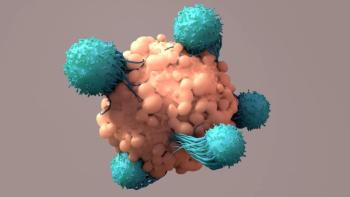
The CAR-T, marketed as Kymriah, showed a 4-year overall survival rate of 79.3% and a median progression-free survival of 53.3 months.
With regard to safety, there were no dose-limiting toxicities, no cases of GvHD, and no cases of TAK-007-related ICANS.

The Medical Director of Pediatric Hematology/Oncology at Sarah Cannon Research Institute discussed the latest data update from the CLIMB SCD-121 trial evaluating exa-cel.

Protocol-defined transfusion independence (TI) was achieved by 52 of the 63 patients in long-term follow-up study LTF-303.

Allo-HSCT showed good 2-year survival data, with matched sibling donors showing superior outcomes to alternative donors.

In the wake of fludarabine shortages, lemphodepletion with bendamustine was found to be an effective alternative compared for patients with large B-cell lymphoma being treated with a CD19-directed CAR T-cell therapy.

With an FDA deadline pending in January, tabelecleucel remained safe and effective with longer follow-up for Epstein–Barr virus-associated post-transplant lymphoproliferative disease.

Zamtocabtagene autoleucel showed promising early complete response rates and survival outcomes in patients with relapsed/refractory diffuse large B-cell lymphoma.
Rapcabtagene autoleucel showed high rates of durable complete remissions and a favorable safety profile for patients with relapsed/refractory diffuse large B-cell lymphoma.

The professor of pediatric hematology/oncology at CS Mott Children’s Hospital discussed a sub analysis of the HOPE-B trial.

The assistant professor at Mayo Clinic School of Medicine shared her outlook and predictions on research with T-cell lymphomas.

The professor of medicine at Baylor College of Medicine discussed research with NK-T cells and alternatives to αβ T-cells.

The assistant professor at Mayo Clinic School of Medicine discussed plans for further research and a phase 2/3 study.

The assistant professor at Mayo Clinic School of Medicine discussed the design of the phase 1 trial.

The clinical assistant professor at Stanford Medicine discussed potential applications for machine learning in analyzing data in medicine.

The clinical professor in the Department of Human Genetics at University of Texas Rio Grande Valley discussed how a personalized gene editing approach may help patients avoid development of FVIII inhibitors.

The internal medicine resident physician at University of Kansas Medical Center also discussed highlights from the ASH 2023 meeting.

The clinical assistant professor at Stanford Medicine also shared his excitement on the recent approvals of lovo-cel and exa-cel.

The associate professor at Fred Hutch Cancer Center discussed trends he observed in the field in 2023 and at ASH 2023.

The postdoctoral researcher at Laboratory for Translational Cancer Immunology, Ludwig-Maximilians-Universität München, discussed research he was excited to see at ASH 2023 and in the field in general.