
The FDA has approved nivolumab as a treatment for patients with metastatic renal cell carcinoma following prior treatment with an anti-angiogenic therapy.

The FDA has approved nivolumab as a treatment for patients with metastatic renal cell carcinoma following prior treatment with an anti-angiogenic therapy.

A pilot study of the efficacy of CAR T-cell therapy in patients with EGFRvIII-positive glioblastoma multiforme (GBM) has generated encouraging findings.
Though clinical work is ongoing and early, researchers are already considering how to manage potentially fatal neurotoxicities in patients treated with chimeric antigen receptor T-cell therapy

The discovery of a possible trigger for PD and Lewy body dementia could provide a new avenue for gene therapy in these neurological conditions.
The FDA has granted a breakthrough therapy designation to avelumab as a potential treatment for patients with metastatic Merkel cell carcinoma following progression on at least one prior chemotherapy regimen.

The FDA has assigned a priority review designation to the PD-1 inhibitor nivolumab as a treatment for patients with advanced renal cell carcinoma following prior antiangiogenic therapy.

A phase III gene therapy trial for Leber congenital amaurosis showed that patients’ mean mobility test scores promptly improved after treatment, and the benefit was sustained at 1 year, said Albert M. Maguire, MD.

The FDA has granted an accelerated approval to osimertinib for patients with advanced EGFR T790M mutation positive non–small cell lung cancer following prior therapy on a prior EGFR TKI.
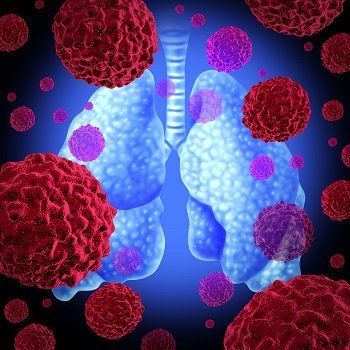
Advanced lung cancer patients who have tumors with mutations in the epidermal growth factor receptor (EGFR) gene may benefit from the combination treatment of erlotinib standard therapy plus tivantinib.

The targeted therapy, nivolumab (Opdivo, Bristol Myers Squibb), improved median overall survival by 5.4 months among patients with previously treated renal cell carcinoma (RCC) compared to standard of care everolimus (Afinitor).

A research team in the UK looked at how well rituximab (Rituxan/Genentech) improved the Sjogren's Syndrome symptoms of fatigue and dry mouth.

The combination of lenalidomide and rituximab demonstrated an objective response rate of 92% as initial therapy for patients with mantle cell lymphoma.

After melanoma and non-small cell lung cancer, the FDA has granted Breakthrough Therapy status to pembrolizumab in advanced colorectal cancer patients with mismatched repair deficiency.

The FDA has granted a breakthrough therapy designation to pexidartinib as a potential therapy for patients with tenosynovial giant cell tumor for which surgical removal is contraindicate.

Patients with renal cell carcinoma whose disease progressed after previous VEGF therapy saw increased delays in disease progression when treated with lenvatinib.

In patients with chronic myeloid leukemia (CML), a prospective, long-term study has found that hematopoietic stem cell transplantation (HSCT) and drug therapy yielded similar 10-year survival outcomes.

Rolling submission of a new drug application for cabozantinib has been initiated for patients with advanced renal cell carcinoma who have received one prior therapy.

It wasn't long ago that researchers first identified a piece of DNA that regulates cholesterol. This gene has been recently developed into a cholesterol-lowering agent and it's time to address where we go from here.

Researchers in Germany appear to have identified a gene-expression signature associated with metastasis in sporadic medullary thyroid cancer and prognostic molecular tumor markers of medullary thyroid cancer response to vandetanib therapy.

The IMA901 multipeptide vaccine added to sunitinib failed to improve outcomes versus sunitinib alone as first-line therapy for advanced/metastatic renal cell carcinoma.

Live cell therapy--an unproven treatment involving injections of live fetal cells from sheep--is legal in Germany. A group of New Yorkers who went there to make them younger and healthier got Q fever instead, the CDC reports.

The heterogeneity of mantle cell lymphoma will require new combination strategies to improve outcomes.

Nivolumab (Opdivo) has received an FDA breakthrough therapy designation for the treatment of patients with advanced renal cell carcinoma.

The advent of gene therapy poses a new area of drug development for inherited and acquires ocular disorders.
Radiation therapy with concurrent chemotherapy is an effective treatment strategy for small-cell bladder cancer.

Melanoma and other types of skin cancer are among the many types of cancer poised to benefit greatly from genomic research that identifies susceptibilities and potential targets for genetic-based therapy. A recent paper in Pigment Cell & Melanoma Research suggests, however, that an entire category of genetic mutations – one that could be incredibly fruitful in terms of diagnosis and treatment – is largely being ignored.

The third-generation TKI osimertinib (AZD9291) showed a 71% objective response rate in patients with EGFR T790M-mutant non–small cell lung cancer following resistance to frontline anti-EGFR therapy.

Coexisting driver mutations in EGFR-mutant non–small cell lung cancer could potentially contribute to primary resistance to EGFR-targeted therapy.

California researchers report good results in a phase II study of a gene therapy for congestive heart failure. The news comes five months after Celladon's Mydicar gene therapy for CHF failed to meet its trial's endpoints.

A chemotherapy-free regimen of nivolumab and ipilimumab demonstrated activity as a first-line therapy for patients with advanced non–small cell lung cancer.