
The CD19-targeted CAR T-cell product axicabtagene ciloleucel (axi-cel; Yescarta) is currently being investigated in patients with relapsed/refractory MCL in the ongoing ZUMA-2 trial.

The CD19-targeted CAR T-cell product axicabtagene ciloleucel (axi-cel; Yescarta) is currently being investigated in patients with relapsed/refractory MCL in the ongoing ZUMA-2 trial.

Several studies presented at the 2018 ASCO Annual Meeting helped further refine and inform treatment strategies for the budding class of CAR T-cell therapies, with a focus on predicting adverse events and optimizing efficacy.
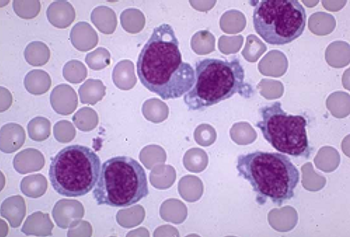
A study recently published in Cell investigated the deletion of the CD33 protein to enable CAR T-cells to more accurately target and attack cancerous cells in patients with n acute myeloid leukemia (AML).
The FDA has granted a Breakthrough Therapy designation to bluebird bio, Inc’s Lenti-D, a gene therapy for patients with cerebral adrenoleukodystrophy, an X-linked genetic disorder caused by a defect in the gene ABCD1.

In TRANSCEND NHL 001, the CD19-directed 4-1BB CAR T-cell product lisocabtagene maraleucel yielded durable responses in heavily pretreated R/R DLBCL.

At the 2018 American Society of Clinical Oncology Annual Meeting, June 1-5, Chicago, Illinois, Noopur S. Raje, MD, director, Center for Multiple Myeloma, Massachusetts General Hospital Cancer Center, presented results from the phase 1 multicenter study with a second-generation chimeric antigen receptor (CAR) T-cell therapy called bb2121.

Therapy with CAR T cells may benefit patients with highly refractory multiple myeloma, said U Penn’s Adam Cohen at ASCO 2018.

Marijke van den Berg, MD, PhD, Alok Srivastava, MD, and Glenn Pierce, MD, PhD discuss gene therapy in hemophilia.
The FDA has granted crizotinib a breakthrough therapy designation for the treatment of patients with metastatic non–small cell lung cancer with MET exon 14 alterations, and for use in patients with relapsed/refractory ALK+ anaplastic large cell lymphoma.

Supported by positive data from an ongoing Phase 2/3 study, bluebird bio’s Lenti-D has been granted Breakthrough Therapy designation by the US FDA for the treatment of patients with cerebral adrenoleukodystrophy.

Novel combination regimens anchored by pembrolizumab (Keytruda), atezolizumab (Tecentriq), or nivolumab (Opdivo) are opening the door to new options and an opportunity to personalize therapy in non–small cell lung cancer.
New data demonstrates clinical benefit in hemophilia B patients with pre-existing anti-AAV5 neutralizing antibodies.

Anas Younes, MD, discusses the current and future state of CAR T-cell therapies and immune checkpoint inhibitors in the landscape of hematologic malignancies.

The phase 1/2 trial for ABO-102 (AAV-SGSH), clinical gene therapy for the treatment of Sanfilippo syndrome type A (MPS III A) shows efficacy in trial update.

SL-401, a novel therapy that targets a cancer stemness pathway, is being investigated in patients with blastic plasmacytoid dendritic cell neoplasm in a phase I/II trial.

The FDA has granted Rare Pediatric Disease Designation to Myonexus Therapeutics for its MYO-101, which is an AAV-based gene therapy for the treatment of limb girdle muscular dystrophy (LGMD) type 2E.

CMS's initial payment codes for CAR T-cell therapies are opposed by the medical community on the basis that they would be cumbersome to implement and wouldn't reflect the full amount of care delivered to each patient.

The US Food and Drug Administration (FDA) has accepted the Bioverativ's Investigational New Drug (IND) application for BIVV003, a gene-edited cell therapy candidate for the treatment of people with sickle cell disease.

The investigational new drug application allows the initiation of phase 1/2 clinical trial to assess the safety of BIVV003 in adults.

Agilis Biotherapeutics, Inc. has announced that the company's gene therapy for AADC deficiency results in de novo dopamine production and supports durable Improvement in major motor milestones.

New data being presented at ASGCT detail patients (1.67 to 8.42 years of age) enrolled in a study evaluating the investigational gene therapy treatment, AGIL-AADC.
The first patient has been dosed in aphase 1/2 study (BMN 270-203) evaluating the investigational gene therapy, valoctocogene roxaparvovec, in severe hemophilia A patients with pre-existing AAV5 antibodies.

A new case study found that an acute myeloid leukemia patient has remained cancer free for 9 months following treatment with the chimeric antigen receptor (CAR) T-cell treatment, CYAD-01, and a bone marrow transplant.

The approval includes adults with R/R DLBCL after two or more lines of prior systemic therapy, high-grade B-cell lymphoma, and DLBCL arising from FL.

A first-time study of chimeric antigen receptor T-cell therapy in youths with Down syndrome-associated relapsed/refractory (r/r) acute lymphoblastic leukemia produced high remission rates and toxicity results that were similar to those observed in patients with r/r ALL.

Results from a recent study may show why some patients with chronic lymphocytic leukemia are resistant to tisagenlecleucel, while potentially offering a pathway to enhance patient response.

Orchard Therapeutics announced that its gene therapy candidate, OTL-200, has been granted Rare Pediatric Disease designation for the treatment of metachromatic leukodystrophy.

CAR T-cell therapy can induce next generation sequencing negativity in patients with relapsed/refractory acute lymphoblastic leukemia, suggesting a "synergistic" relationship with hematopoietic cell transplant.

Tisagenlecleucel, sold as Kymriah, has gained its second indication following the FDA's approval of the chimeric antigen receptor T-cell therapy for the treatment of adult patients with relapsed or refractory large B-cell lymphoma, the most common form of non-Hodgkin lymphoma.

REGENXBIO Inc. announced that the U.S. FDA has granted Fast Track designation to RGX-131, a novel, one-time investigational treatment for mucopolysaccharidosis type II (MPS II).