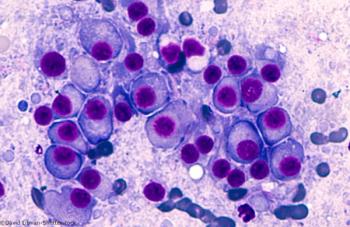
The FDA has granted a priority review designation to a supplemental biologics license application for pembrolizumab (Keytruda) as a treatment for patients with advanced small cell lung cancer whose disease has progressed following ≥2 prior lines of therapy.