The CAR T-cell therapy elicited a 92% ORR, with high rates of durable responses in patients with indolent non-Hodgkin lymphoma.
The CAR T-cell therapy elicited a 92% ORR, with high rates of durable responses in patients with indolent non-Hodgkin lymphoma.
The enriched chimeric antigen receptor T-cell therapy improved responses and prolonged duration of response in patients with relapsed/refractory multiple myeloma.
A novel CD20xCD3 bispecific antibody, odronextamab, continues to show intriguing antitumor activity and an acceptable safety profile in patients with relapsed/refractory B-cell non-Hodgkin lymphoma, including those who have previously received chimeric antigen receptor T-cell therapy.
Treatment with the CAR T-cell therapy ciltacabtagene autoleucel led to a high response rate and an acceptable safety profile at the recommended phase 2 dose in patients with relapsed or refractory multiple myeloma.

December 5, 2020 - Treatment with the CAR T-cell therapy ciltacabtagene autoleucel led to a high response rate and an acceptable safety profile at the recommended phase 2 dose in patients with relapsed or refractory multiple myeloma.

December 5, 2020 - Engineering chimeric antigen receptors T cells to overcome CD58 loss may provide a path forward for patients with large B-cell lymphomas who do not respond to treatment with immunotherapy.
The effector profile of the SARS-CoV-2 virus–specific T-cell therapy, ALVR109, was polyclonal, polyfunctional, and displayed cytolytic activity against viral targets without allogeneic or autologous reactivity, suggesting ALVR109 could be a safe and effective treatment for the coronavirus disease 2019.

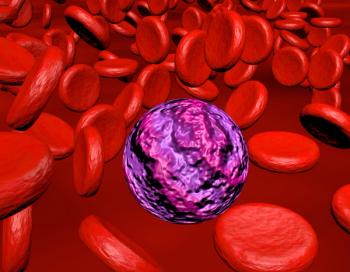
ALLO-715, an off-the-shelf chimeric antigen receptor T-cell therapy that targets B-cell maturation antigen, elicited responses in heavily pretreated patients with relapsed/refractory multiple myeloma in early findings from a first-in-human study presented at the 2020 ASH Meeting.

December 5, 2020 - The enriched chimeric antigen receptor T-cell therapy bb21217 improved responses and also prolonged duration of response compared with non-enriched CAR T cells in patients with relapsed/refractory multiple myeloma.

December 5, 2020 - Patients with heavily pretreated multiple myeloma maintained durable responses with the chimeric antigen receptor T-cell therapy idecabtagene vicleucel in updated findings presented from the phase 1 CRB-401 trial.

December 5, 2020 - The CAR T-cell therapy axicabtagene ciloleucel demonstrated long-term disease control with rapid responses and robust CAR T-cell expansion among patients with refractory large B-cell lymphoma.
Results were released for a leading chimeric antigen receptor (CAR) T-cell therapy candidate in multiple myeloma, along with long-term findings for an early treatment that may soon face competition.
A preview of the 62nd annual American Society of Hematology meeting, taking place in a virtual format.
The efficacy of the novel intravesical gene-mediated therapy nadofaragene firadenovec was sustained across subgroups of patients with high-grade, BCG-unresponsive non-muscle invasive bladder cancer.
December 3, 2020 — The survivin-targeted T-cell therapy DPX-Survivac, when used in combination with intermittent low-dose cyclophosphamide, prolonged clinical benefit with promising tolerability in patients with recurrent, advanced platinum-sensitive and -resistant ovarian cancer.

A pooled analysis compared survival among patients with metastatic renal cell carcinoma treated with cytoreductive nephrectomy and either targeted therapy or immunotherapy regimens utilizing checkpoint inhibitors.
The study evaluated lurbinectedin (Zepzelca) in combination with doxorubicin versus physician's choice of topotecan or cyclophosphamide/doxorubicin/vincristine for adult patients with small cell lung cancer whose disease progressed following 1 prior platinum-containing line of therapy.

December 2, 2020 - Patients with high-grade Bacillus Calmette-Guérin unresponsive non-muscle invasive bladder cancer who responded to the investigational gene therapy nadofaragene firadenovec had a lower rate of cystectomy and delayed time to cystectomy compared with those who did not respond.

November 30, 2020 - The FDA has granted a breakthrough therapy designation to zanidatamab for the treatment of patients with HER2 gene–amplified biliary tract cancer who have received prior therapy.

Penn Medicine researchers use mice experiments to find a potential solution to the challenge of delivering CAR T cell treatments to solid tumors in glioblastoma.
The compiled results revealed that hepatotoxicity related to the gene therapy typically presented as cholestatic, which could be prophylactically treated with prednisolone.

Alan P. Z. Skarbnik, MD, highlights how treatment decisions in mantle cell lymphoma have become more nuanced since the FDA approval of the CAR T-cell therapy brexucabtagene autoleucel in the relapsed/refractory setting.

Olalekan O. Oluwole, MBBS, MD, discusses the approvals of tisagenlecleucel and axicabtagene ciloleucel, along with several research efforts that have been dedicated to the development and exploration of CAR T-cell therapies in the realm of leukemias and lymphomas.

City of Hope's Dr. Tanya Siddiqi offers an update on a new chimeric antigen receptor (CAR) T-cell therapy awaiting approval from the FDA.
November 24, 2020 - Until now, the field of cell-based immunotherapy has been dominated by chimeric antigen receptor (CAR) T cells, with groundbreaking FDA approvals for 3 drugs across several types of hematologic malignancies. In solid tumors, however, CAR T-cell therapies have yet to gain ground.

Ronald Crystal, MD, chairman, Department of Genetic Medicine, Weill Cornell Medicine, discussed the promise of gene therapy for patients with Alzheimer disease and related disorders.

These study results suggest that osimertinib as adjuvant therapy is an effective treatment strategy for patients with stage IB to IIIA EGFR-positive non-small cell lung cancer following complete tumor resection.

A new report finds including rituximab in first-line therapy for diffuse large B-cell lymphoma (DLBCL) results in better overall outcomes that more than offset the higher initial cost of therapy.

The FDA approved a 1500 mg fixed dose of durvalumab (Imfinzi) administered every 4 weeks for the treatment of unresectable stage III non-small cell lung cancer after chemoradiation therapy and previously treated advanced bladder cancer.

Joshua Brody, MD, discusses advances made with CAR T-cell therapy in MCL, the promise of venetoclax in B-cell malignancies, and the potential for bispecific antibody combination regimens in this disease.