
Novartis and the Bill & Melinda Gates Foundation have entered a new agreement to discover and develop a single-administration gene therapy to cure sickle cell disease in countries with limited healthcare infrastructure.

Novartis and the Bill & Melinda Gates Foundation have entered a new agreement to discover and develop a single-administration gene therapy to cure sickle cell disease in countries with limited healthcare infrastructure.

Yi Lin, MD, PhD, discusses promising data with CAR T-cell therapy in multiple myeloma.

Novartis is teaming up with the Gates Foundation to develop a gene therapy for sickle cell disease; the World Health Organization reports a drop in global cases of coronavirus disease 2019 (COVID-19); storms hinder vaccine rollout across the United States.

On this episode of Managed Care Cast, we highlight a new feature on AJMC.com, the website of The American Journal of Managed Care®, called Clinical Spotlight, where our editors provide a series of interviews with leading experts in certain specialties.

The suspension is due to recently reported diagnoses of AML and myelodysplastic syndrome in 2 treated patients.

No approved treatment for leber hereditary optic neuropathy is currently available in the United States.
CAR T-cell therapy has shown robust responses and curative potential in patients with diffuse large B-cell lymphoma, regardless of cytogenetics or age.

February 15, 2021 - Betibeglogene autotemcel, a one-time gene therapy, enabled durable transfusion independence in most patients with transfusion-dependent β-thalassemia who were treated across 4 clinical studies.

Both therapeutic programs utilize AAD2-GDNF gene therapy targeted to brain structures vulnerable to Parkinson disease and multiple system atrophy.
Descriptive findings from the phase 1/2 study allude to promise for the gene therapy in the rare pediatric disorder.

New phase 2/3 findings meet investigators' hypotheses on the gene therapy's mixed benefits for heparan sulfate reduction.

The AAV-based gene therapy was well-tolerated and showed enough promising effect to warrant further investigation, researchers reported.

Investigators observed sustained, dose-dependent benefits for young patients at 24 months.

Treatment with the first-generation precision cell therapy Orca-T led to a significant reduction in cases of graft-versus-host disease, an impressive GVHD relapse-free survival rate, a lack of treatment-related mortalities, while showcasing scalability potential.
Study examining the role of IL-17A in patients with diabetes.
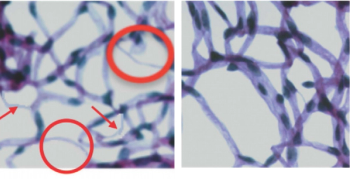
The HSPC therapy showed fetal hemoglobin production in transfusion-dependent patients in a matter of months—with sustained results over 1 year.

Treatment with the investigative gene cell therapy betibeglogene autotemcel led to durable transfusion independence in 87% of pediatric patients less than 18 years of age with transfusion-dependent beta-thalassemia with a median average hemoglobin of 11.3 g/dL.
Investigators focus on biophysical method to study protein-protein interactions .
Responsiveness to treatment received immediately prior to CAR T-cell therapy may not be associated with post–CAR T outcomes in patients with relapsed/refractory diffuse large B-cell lymphoma who receive axicabtagene ciloleucel.

The investigators found the primary efficacy endpoints occurred in 20 evaluable patients (87%).

FLT201 is a combination of AAVS3 capsid and a liver-specific promotor to drive the expression of GCasevar85.
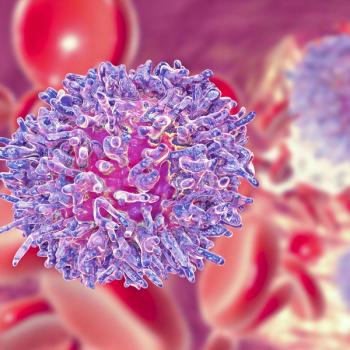
Patients with refractory large B-cell lymphoma have less to gain from axicabtagene ciloleucel if they have never achieved a complete response to any line of prior therapy.

Data from the ongoing HGB-206 study reports reduced hemolysis, increased total hemoglobin, and a complete resolution of vaso-occlusive crises among patients.

New WORLDSymposium findings show a treated patient had 100% reduction in the accumulating fatty substrate associated with the burdensome rare disease after 1 year.

Prior exposure to anti-CD19 therapy did not impact response to the CAR T-cell therapy lisocabtagene maraleucel in patients with relapsed/refractory large B-cell lymphoma.
These findings may have implications for patients with hematologic malignancies, suggesting the development of protective memory against SARS-CoV2 and non-SARS human coronaviruses.

February 5, 2021 - Following stem cell transplant or treatment with CAR T-cell therapies, patients with hematologic malignancies and coronavirus disease 2019 tend to have favorable outcomes, especially if they are diagnosed in complete remission and further out from their cell infusion.

A CAR T-cell therapy that promises fewer side effects, and possibly lower hospital costs, wins approval after lengthy delays.

The 1 patient who did not received immunomodulatory agents demonstrated the highest level of FVIII activity.
Although safety remains a concern with gene therapy, investigators are breaking ground in cell and gene therapy, and many believe that ultimately, a string of cured cancers will follow.