
February 3, 2021 - The combination of ceralasertib plus durvalumab improved overall response rate in patients with non‒small cell lung cancer who progressed on an anti-PD-1/PD-L1 therapy.

February 3, 2021 - The combination of ceralasertib plus durvalumab improved overall response rate in patients with non‒small cell lung cancer who progressed on an anti-PD-1/PD-L1 therapy.

Neil Berinstein, MD, discussed the early promise with this T-cell therapy in relapsed/refractory diffuse large B-cell lymphoma.

Neurocrine Biosciences and Voyager Therapeutics have terminated the Parkinson disease portion of their partnership, ending development for VY-AADC, also known as NBIb-1817.

A substantial proportion of patients with inherited retinal disease could be treated with base editing, while therapeutic strategies that focus on common variants could be used to treat a large number of patients with the disease, according to study results.

Clinically relevant scores of 32 and 44 on the Fugl-Meyer Motor Score were documented in 2 patients who received NSI-566.
An engineered lentivirus was created to avoid some of the drawbacks associated with current gene therapy vectors for sickle cell disease (SCD) and beta-thalassemia.

January 28, 2021 — Frontline pembrolizumab continued to demonstrate clinically meaningful improvements in overall survival, overall response rate, and time to progression on next-line therapy compared with platinum-based chemotherapy in patients with locally advanced or metastatic PD-L1–positive non–small cell lung cancer without sensitizing EGFR or ALK mutations.

While these therapies continue to revolutionize the treatment landscape of SMA, treatments are not without shortcomings or challenges.

Two gene therapy techniques in separate, concurrently published trials demonstrate clinical success in mitigating monogenic hemoglobinopathies.

The FDA has granted Fast Track designation to MeiraGTx's AAV-CNGA3 gene therapy product candidate for the treatment of achromatopsia (ACHM).
January 22, 2021 — The Japan Ministry of Health, Labour and Welfare has approved the CAR T-cell therapy axicabtagene ciloleucel for use in the treatment of adult patients with certain relapsed/refractory large B-cell lymphomas.
Exciting new and ongoing developments in chimeric antigen receptor (CAR) T-cell therapies were covered at the 62nd American Society of Hematology (ASH) annual meeting.

Neurophth Therapeutics, Inc (Neurophth) and AAVnerGene Inc have announced the launch of a strategic partnership that will grant Neurophth global rights to mutually select adeno-associated virus (AAV) capsids for the creation of the next-generation ophthalmic gene therapy.

The researchers unexpectedly found sustained visual improvement in both eyes, despite only 1 eye being treated with AAV.

In our exclusive interview, Dr. Kansagra, Dr. D’Souza, and Dr. Dholaria provided an in-depth look into the current state of cellular therapy in hematologic malignancies, the benefits and drawbacks of approved and investigational products, and new constructs for CAR T in multiple myeloma and lymphoma.
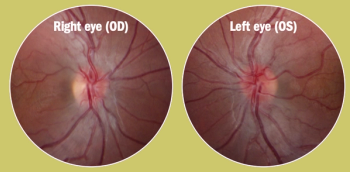
A new gene therapy for this patient population targets the ND4 gene mutation.

The Pfizer candidate PF-06939926 has also received fast track, orphan drug, and rare pediatric disease designations from the FDA.

FDA accepts for priority review a Biologics License Application for V114, Merck's investigational 15-valent pneumococcal conjugate vaccine; bluebird bio will be split into 2 publicly traded drug companies; a new variant of coronavirus is reported in Japan.
There was no statistically significant difference between treatment-related adverse events in the SB623 stem cell and control groups.

New one-year data makes history as the first to indicate the superiority of a one-injection gene therapy versus Factor VIII prophylaxis.

Two teams of researchers from Gyroscope Therapeutics and the University of Pennsylvania are joining forces to explore gene therapy targets for three specific serious eye diseases.
The Expanded Access Program will offer treatment for patients with ALS who have completed the phase 3 clinical trial and will not interfere with data or regulatory timelines.

Minimal fat infiltration was observed on MR images from the SRP-9001 arm compared to participants from the natural history cohort.

ViGeneron and Biogen this week have announced a global collaboration and licensing agreement in which the partners will develop and commercialize gene therapy products based on adeno-associated virus (AAV) vectors that treat inherited eye disease.

James Gerson, MD, discusses the introduction of CAR T-cell therapy to the mantle cell lymphoma armamentarium and how induction therapy followed by stem cell transplant has maintained a role.

Genentech's tiragolumab, a novel immunotherapy for non-small cell lung cancer with PD-L1 expression, is the first anti-TIGIT therapy to be granted Breakthrough Therapy Designation.
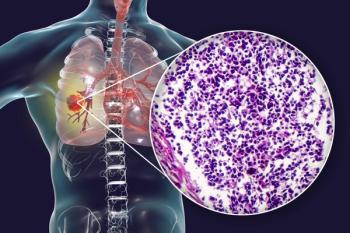
Nivolumab was previously granted accelerated approval by the FDA for the treatment of patients with small cell lung cancer (SCLC) whose disease had progressed after platinum-based chemotherapy and at least 1 other line of therapy, but phase 3 trial results led to a decision to withdraw the indication.
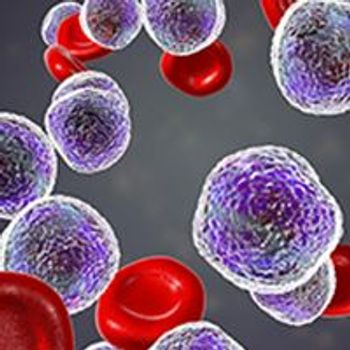
January 4, 2021 - The biologics license application for the CAR T-cell product lisocabtagene maraleucel in adult patients with relapsed/refractory large B-cell lymphoma following at least 2 previous therapies continues to be under regulatory review by the FDA, and a decision on the application has not yet been reached.

Nine pediatric patients with Leber congenital amaurosis show visual improvement in clinical trials.