
After a more than 35-year pursuit, the licensing of a gene therapy product for treating hemophilia may be available within 2 years.

After a more than 35-year pursuit, the licensing of a gene therapy product for treating hemophilia may be available within 2 years.

The gene therapy SAR439483 demonstrated promising early signs of activity in patients with Leber congenital amaurosis caused by biallelic mutations in GUCY2D.

Nilanjan Ghosh MD, PhD, highlights progress made with CAR T-cell therapies in B-cell lymphoma and some ongoing trials generating interest in the field.

The FDA granted a Regenerative Medicine Advanced Therapy designation to the allogeneic chimeric antigen receptor T-cell therapy as a potential treatment for patients with relapsed/refractory multiple myeloma.

The FDA approval of brexucabtagene autoleucel established CAR T-cell therapy as a treatment option for patients with relapsed/refractory mantle cell lymphoma.
In an AAN plenary talk, Mark H. Tuszynski, MD, PhD, detailed the work he and colleagues have done to push stem cell therapy from the lab to the clinic to improve care for spinal cord injury.

The FDA has granted a fast track designation to LX1001 as a potential treatment for adult patients with APOE4-associated Alzheimer disease.

Vertex Pharmaceuticals will take the lead on worldwide development, manufacturing, and commercializing of CTX001, with payments and split economics to CRISPR Therapeutics.

Betibeglogene autotemcel is being withdrawn from the German market following a breakdown in reimbursement conversations, which has resulted in bluebird reducing and reshaping its European workforce.

Given that some patients may need to travel out of state to access CAR T sites of care, some may not have a clear understanding of their insurance benefits, including requirements for out-of-state or out-of-network treatment, as well as adequate assistance with the costs of medical-related travel.

Three cell and gene therapies were among the drugs included in a specialty drugs pipeline forecast at the Academy of Managed Care Pharmacy 2021 meeting.
In a phase 1 study of the innate cell engager AFM13 pre-complexed with NK cells, all 4 patients with CD30-positive, relapsed/refractory Hodgkin lymphoma treated with the therapy achieved at least a partial response.

Saad Z. Usmani, MD, FACP, discusses the rapidly changing cellular therapy paradigm in relapsed/refractory multiple myeloma.

The first patient has been enrolled and treated with RGX-121 in the third cohort of a phase 1/2 study for patients up to 5 years old with severe MPS II.

RP-L201 continued to show promising preliminary efficacy for patients with severe LAD-I after additional follow-up in a phase 1/2 study.
The FDA has granted an orphan drug designation to CYNK-001 as a potential treatment for adult patients with recurrent glioblastoma multiforme.

Studying zebrafish helps unravel the mysteries of photoreceptor regeneration.
Lifileucel elicited objective responses, including complete responses, for a median duration that was not yet reached at 28.1 months for patients with advanced melanoma.

Studies are uncovering a range of potential treatment options for disorders.
CD19-directed CAR T-cell therapy brexucabtagene autoleucel will be considered by FDA for indication in adults with B-cell precursor acute lymphoblastic leukemia.
Daratumumab appears to be safe when used as consolidation therapy in patients with multiple myeloma, even soon after autologous stem cell transplant, and the agent has also demonstrated early efficacy in the setting of very good responders.
The rolling submission of a biologics license application to support the approval of the investigational BCMA-directed CAR T-cell therapy ciltacabtagene autoleucel for the treatment of patients with relapsed/refractory multiple myeloma has been completed.
Physician offers patient counseling pearls for selected retinal diseases.

AAV2 TrkB-2A-mBDNF resulted in early signs of efficacy in preclinical studies of glaucoma and humanized tauopathy, which could be translatable to other neurodegenerative polygenic disorders.

As more therapies continue to be approved, efforts will focus on toxicity prevention and mitigation strategies for associated unique and potentially life-threatening adverse reactions.

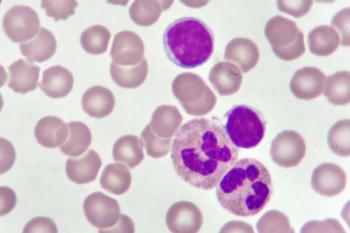
The multitumor-associated antigen-specific T-cell product MT-401 is under investigation as a potential treatment option for patients with acute myeloid leukemia following allogeneic stem cell transplant in both the adjuvant and active disease settings.

CAR T-cell therapies are now incorporated into National Comprehensive Cancer Network guidelines as a recommended third-line strategy in this setting, with the most recent addition being lisocabtagene maraleucel.

The Canada Foundation for Innovation has awarded C$5,187,685 to the Canadian Cancer Trials Group at Queen’s University in Kingston, Ontario, Canada, to fund the infrastructure for a new research platform to coordinate the development of new cancer cell therapies.

Enrollment has completed for the phase 3 GEM-3 study for beremagene geperpavec for patients with dystrophic epidermolysis bullosa. Topline results are anticipated before the end of 2021.

Novel gene therapy demonstrates improved visual acuity and retinal thickness.